
By now, you will probably have had or be about to have your Booking-In appointment with the hospital.
Part 1: This stage in your pregnancy

Gestational Diabetes Mellitus (GDM) is a form of diabetes that may occur during pregnancy. It is the fastest growing type of diabetes in Australia, affecting thousands of pregnant women. It usually occurs, around the 24th to 28th week of pregnancy.
Most of those who develop GDM will no longer have it after their baby is born. However, some will continue to have high blood glucose levels after having their baby.
GDM is diagnosed when higher than normal blood glucose levels appear during pregnancy. For this reason, we recommend testing for gestational diabetes at 26-28 weeks of pregnancy (unless you already have diabetes). If you have risk factors for gestational diabetes, you should be tested earlier in your pregnancy.
For your glucose tolerance test you must:
- bring your pathology slip with you to the hospital (provided at previous appointment)
- fast from midnight the night before - this means no eating, no chewing food or gum and no smoking. You may drink water only during this period.
The testing process:
- your first blood test is taken
- you will then be given a glucose drink supplied by our pathology department
- continue to fast as two more blood tests are required. These are taken an hour after having the drink and again an hour later.
This test will take approximately two hours. You must remain in the hospital until your test is finished.
Our website has more information about gestational diabetes.
Part 2: Things to consider


You may feel very well during your pregnancy, or you may feel irritated or quite unwell. Most discomforts in pregnancy are normal and manageable.
If you are worried about your symptoms, talk to your midwife or doctor as you may need medicine or treatment. If your symptoms become severe, call the hospital immediately.
This section covers many common concerns during pregnancy. We may not cover all of your worries, but we will cover those most asked about.
Our Coping with common pregnancy-related discomforts fact sheet covers more, including morning sickness, constipation, vaginal thrush and more.

There are many factors that can affect your sleep during pregnancy. They can make falling asleep or staying asleep difficult.
These may include:
- nausea
- vomiting
- breast tenderness
- increased heart rate
- shortness of breath
- higher body temperature
- frequent trips to the bathroom overnight
- leg cramps.
More information on sleep in pregnancy including sleep problems and strategies to assist better sleep.


When you are pregnant, dental care is important because hormonal changes can lead to tooth decay and gingivitis (where gums become red, swollen and bleed easily). Gum disease or bacterial infection in the gums has been linked with premature and low-birth-weight infants.
Good dental health before you get pregnant means that you are less likely to need treatment during pregnancy. If you have a dental emergency during pregnancy you might need to have an X-ray. These days X-ray machines emit tiny doses of radiation and are directed at a highly localised area. They are generally safe in pregnancy, but always let your dentist know you are pregnant.
If you are pregnant and have a Medicare card, you do not have to go on a waiting list for dental care in Victoria.
More information on Dental care during pregnancy.

Immunisations:
Check with your doctor that your immunisations are up to date. These include measles, mumps, rubella, chickenpox, diphtheria, tetanus, whooping cough, influenza (flu) and COVID -19. Your doctor can order a blood test to check your level of protection.
The National Immunisation Program Schedule lists a series of immunisations given at specific times from birth through to adulthood.
Vaccinations:
The influenza (flu), pertussis (whooping cough), and COVID-19 vaccines are recommended for all pregnant women.
- Flu symptoms, such as a high temperature, may be harmful for you and your baby. You can have a flu vaccination before or during pregnancy, especially if you are pregnant in the flu season. Pneumococcal vaccine is also recommended for women with risk factors (smokers, for example) when planning pregnancy.
- Whooping cough - This vaccination is strongly recommended between weeks 20 to 32 to protect you and your baby. Immunisation during your pregnancy provides antibodies to protect your baby in their first six months. Partners (if you have one) and close contacts may also consider being vaccinated for their own protection. Several studies of infants with whooping cough show that parents were the main source of infection.
- COVID-19 - This is more dangerous for pregnant women. (Australian Government Department of Health). The best way to reduce your risk is to get vaccinated. Real-world evidence has shown that Pfizer and Moderna vaccines are safe if you are pregnant, breastfeeding or planning pregnancy. You can receive a vaccine at any stage of pregnancy.
More information about COVID-19 vaccine risks, safety, and boosters in pregnancy and while breastfeeding is available from the Australian Government and our COVID-19 Information Hub.
More information about whooping cough and pregnancy and flu.

If you plan to work during your pregnancy, whether it’s right up to the final weeks or finishing several months before your due date, it’s important to make sure that your work environment and the work you do is safe for you and your pregnancy. If you have concerns about your job or your workplace, discuss them with a health professional.
If at any time, your work role or workplace becomes unsafe, your employer should arrange alternative work activities for you while you are pregnant. They should also be able to accommodate you if you return to work while breastfeeding.
Australia has a number of laws to protect you from discrimination in the workplace. Some are specifically related to pregnancy and breastfeeding. It can be helpful to know and understand your rights when discussing any concerns with your employer.
More information about your work rights while pregnant or breastfeeding and paid maternity and parental leave

Wearing seat belts
No matter what stage you are at in your pregnancy, you must always wear a seat belt. By wearing a seat belt, you are protecting yourself and your unborn baby if there is an accident. Remember, it is illegal not to wear a seat belt, unless you have a current medical certificate from your doctor.
When it is no longer comfortable to wear your seat belt over your baby bump, wear the lower belt under it, as explained in this Queensland Government video.
Air travel
The safest time for a well, pregnant woman to travel is after 20 weeks and before 32 weeks.
It’s a good idea to consider the standard of medical care in the country to which you are travelling. In some developing countries, the medical facilities are fewer or of lesser quality than in Australia and the risk of disease is higher. Also, the potential for travel restrictions may keep you in a location for an extended period.
Air travel in the later stages of pregnancy can trigger premature labour. Your midwife or doctor will advise you about travel and vaccinations. Individual airlines may also have policies on pregnancy and travel, so check with your airline before travelling.
While travelling for any lengthy distance by car, plane, boat, or train drink plenty of fluids, move about and stretch your legs often.

Little research is available on the use of hair dyes or hair removers during pregnancy. While they are generally considered safe during pregnancy (very little hair dye is absorbed through the scalp) if you want to be very careful avoid using hair dye or hair removal products in the first three months.
If you do dye your hair when you are pregnant, it might be a good idea to do the following:
- dye your hair in a well-ventilated area to avoid fumes
- go to a hairdresser rather than doing it at home
- wear gloves or ask someone else to apply it for you
- follow the instructions on the package and do an allergy test beforehand.


Baby Friendly Accreditation
At this point you may be thinking about how to feed your baby after they are born.
The Women’s is a Baby Friendly Accredited hospital and follows the World Health Organisation’s 10 steps for successful breastfeeding.
We know that breast milk provides all the nutrition your baby needs for the first six months of life. It also provides a big part of your baby’s nutritional requirements throughout the first year and beyond.
If you choose not to breastfeed or offer breast milk, information on formula feeding will be discussed with you individually, and educational support provided.
The beauty of breastfeeding
During your pregnancy, we will talk with you about how you plan to feed your baby. Your feeding plans, whatever they are, and previous feeding experiences are important.
Whether this is your first baby or you have fed other babies, you may have some questions. Our ‘Your Pregnant, so let’s talk about feeding your baby’ fact sheet is a good place to learn about why breastfeeding is recommended for baby, you and the community.

Placing your baby with their skin on your skin (chest to chest) is important and recommended. The first hour of your baby’s life will assist them to adapt to their new environment. Skin-to-skin contact helps to stabilise and regulate your baby’s temperature, breathing, oxygen levels and heart rate as well as promote breastfeeding instincts.
Our Skin-to-skin care with your baby fact sheet explains more about the many benefits of skin-to-skin care for you and your baby and is available in English, Arabic, Chinese and Vietnamese.


Commencing breastfeeding soon after your baby’s birth guarantees your baby will receive colostrum, 'the first breastmilk'. Colostrum is a nutrient-filled fluid produced before milk is released.
It can help stabilize your baby’s blood sugar levels, boost their newly developing immune system and protect them from illnesses in their first few months.

Room sharing, commonly called ‘Rooming In’, means sharing your sleeping room with your baby. During your stay at the Women’s, you and your baby will most likely stay together.
Having your baby in the same room as you will help you to recognise when your baby is hungry and ready to feed, tired or in need of a cuddle. Rooming In and breastfeeding are also two of the guidelines to help reduce the risk of SIDS, together with providing a safe sleeping space.
Red Nose Australia has more safe sleeping information
At the Women’s Pepi Pods can be used. These are purpose-built plastic tubs that are used as an alternative to standard cots. They enable you to safely share your bed with your baby and can be used if you have a caesarean.
Part 2.3: Physiotherapy and exercise


Exercising within your limits is very good during pregnancy.
As your baby grows:
- your stomach muscles need to be strong to support the baby’s weight
- your leg muscles need extra strength so you can climb stairs and get in and out of cars
- your back needs to be strong to lift and carry
- your pelvic floor muscles need to be strong and work effectively, to avoid them becoming stretched and weakened as your baby grows (More information in the next section)
The best exercise is enjoyable, done in moderation, and something that you can do on most days of the week. Physical activity will help you to stay well, feel positive and cope with the challenges of becoming a parent.
If you were inactive before your pregnancy, it could be harmful to you and your baby to suddenly take up ‘strenuous’ exercise. Seek advice and find out what is appropriate for you.
Our physiotherapists have specialist knowledge about the physical changes that occur during pregnancy. They can assess and treat pregnancy-related back and pelvic pain.
Stop exercising and contact the hospital if you experience any of the following symptoms while exercising:
- dizziness
- vaginal bleeding
- contractions
- pain
- unusual shortness of breath
- headaches or nausea
- decreased baby movements
- ‘waters’ leaking.
More information about exercise in pregnancy and our Physiotherapy Department.
Other certified women’s health physiotherapists can be found on the CFA Physiotherapy Group (Vic) website

Your posture changes during pregnancy. As your baby grows, your abdomen increases in size and shifts your centre of gravity. Without realising it, you may change the way you stand, sit and walk.
It is important to be aware of your posture. Maintain a correct posture while gently tightening your lower abdominal muscles to support the weight of your baby.

One of the most important things you can do during pregnancy to prepare for labour is to stay active and to have a good understanding of your pelvic floor muscles.
The pelvic floor is a group of muscles and ligaments which support the bladder, uterus (womb) and bowel. The openings from these organs - the urethra from the bladder, the vagina from the uterus and the anus from the bowel - pass through the pelvic floor. The pelvic floor muscles attach to your pubic bone at the front and the tail bone at the back and form the base of your pelvis.
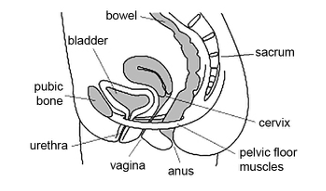
The pelvic floor muscles help to hold the uterus in position. They also play an important role in sexual sensation and function.
Over the course of your pregnancy the pelvic floor muscles stretch and weaken due to the weight of your baby. Some of the hormones involved in pregnancy further loosen and stretch these muscles. It is important to exercise these muscles to keep them as strong as possible and working effectively.
It is also important to avoid constipation and straining on the toilet as this can also weaken your pelvic floor muscles.
Watch our video on how to find and exercise your pelvic floor muscles.
Our Pelvic floor exercises fact sheet includes more information about your pelvic floor muscles and is available in many languages.

Relaxation for life and labour
Now is the best time to learn how to relax. Being relaxed means your muscles are looser, and you’re able to breathe more easily and rhythmically. This keeps your oxygen levels high and your stress hormones low. Being relaxed can help you cope with stress, tiredness and pain.
Using relaxation methods in labour helps to decrease the amount of adrenaline you produce. Adrenaline is a hormone the body produces in response to fear, anxiety and pain. High levels of adrenaline cause us to either fight, flee or freeze.
Relaxation also promotes the production of oxytocin (the hormone that makes labour progress). Being relaxed may also reduce the need for medical options of pain relief.
Learning breath awareness and relaxation techniques will help reduce anxiety and pain in labour and also benefit you after your baby is born.
Pregnancy yoga and pregnancy pilates classes, hypnobirthing techniques, walking, listening to music, tai-chi, breath awareness, mindfulness and mediation are activities that can assist you to relax.
In order to benefit from these activities, it’s important to:
- find an activity that suits you
- practice as much as possible. At least 3-4 times per week and when possible, practice with your birth support person.
The Centre of Perinatal Excellence website includes stress and relaxation strategies in pregnancy.



If you have a partner, you may be concerned that having sex will harm your developing baby. If you have a normal healthy pregnancy and you want to have sex, there is no reason not to. It will not harm you or your baby.
If you don’t want to have sex during pregnancy, you may prefer just to be held, touched, or massaged.
For some, their sexual appetite increases during pregnancy.
Later in pregnancy, sex may not be that easy. You may have to find different positions. This can be a time to experiment and explore together.
Always ask your midwife or doctor for advice if:
- you have any vaginal bleeding (more blood than the size of a 50cent coin)
- you’ve had previous miscarriages
- your waters have broken (there may be a risk of infection to your baby)
- you have had previous premature births or gynaecological problems.
The UK National Health Service website and the Raising Children Network have more information on sexual activity during pregnancy.

Now is a great time to start thinking and talking to your partner or support circle about your needs during your pregnancy, labour and birth, as well as the support required after your baby is born.
Here are some suggestions on how they can become involved:
- attending the clinic or doctor’s visits during the pregnancy and any scans (if restrictions allow this)
- learn together by attending a Childbirth education program, reading, viewing videos from the Women’s website etc
- discuss the roles and distribution of work around the home both now and after the birth
- acknowledge and discuss any relationship changes that may occur with the need to care for a baby, especially in the first weeks and months after baby is born. Pregnancy is a time of big changes as discussed on Raising Children, the Australian Parenting website
- start talking about parenting expectations that you each may have. Consider your own family’s parenting and those skills and traits you would and would not like to use
- discuss return to work expectations and financial planning for at least the next 6-12 months. Find out about entitlements when returning to work from parental leave and requesting flexible working arrangements.
We hope you have found this information helpful.
If you have any health concerns please talk to one of your health care professionals – midwife, General Practitioner (GP), hospital doctor, etc.
There will be more to read and learn next week, in week 23 of your pregnancy. Stay safe and well.