

The Gandel Simulation Service uses translational simulation to improve teamwork, coordination, patient outcomes, and safety at the Women’s.
The service was established at The Royal Women's Hospital in 2019 with funding from Gandel Philanthropy and The University of Melbourne Medical School.
The service uses translational simulation for quality improvement and education with simulations conducted in situ or in the real space with real multi-professional teams and in real time. Simulation is used for education and testing of hospital processes and pathways for all clinical and nonclinical staff with planned consumer engagement. Simulations are also used to test procedures, protocols and prospective new equipment at the Women’s.
The use of simulation helps nurses, midwives, doctors, allied health professionals and all administrative and support staff at the Women’s to prepare for scenarios they may encounter in both clinical and non-clinical settings. This has included preparation for the COVID-19 pandemic and implementation of the electronic medical record or EMR.
A comprehensive research and evaluation program is a key focus of the service to ensure best practice and sustainability. Our priority is helping everyone at the Women's to do their work better together and make work as imagined, work as done.

Download the GSS Handbook - 4th Edition 2022 


The Women’s Maternity Leading High Performance Teamwork Strategy is a multi-faceted program led by Gandel Simulation Service in collaboration with Bond Translational Simulation Collaborative and A/Prof Stuart Marshall. At The Women’s this is in collaboration with clinical directors, clinicians, consumers, the Clinical Education Unit, and the Quality & Safety team.
Download the GSS - Maternity High Performance Teamwork Strategy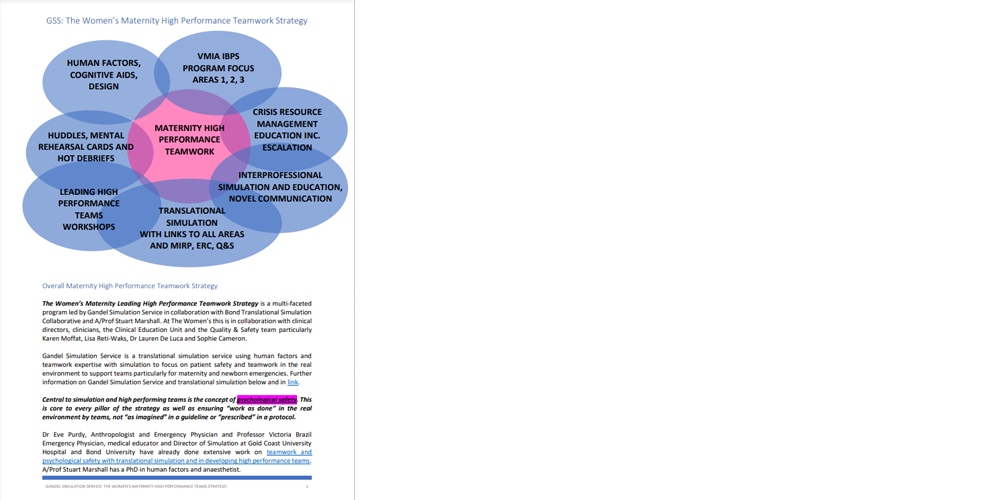

Our core simulation education focus is in the following areas to ensure best practice as well as quality and safety along with our translational testing simulation work.
- Maternity emergency training
- Newborn emergency training
- Medical emergency team training
- Operating theatre team training
- Surgical and other skills training
Our maternity emergency training and approach to culture and teamwork aims to ensure best practice and safety as well as meet targets set by the Victorian Managed Insurance Agency (VMIA) Incentivising Better Patient Safety (IBPS) Program.
About Translational Simulation
What is translational simulation?
Translational simulation is a type of healthcare simulation focused directly on improving patient care and healthcare systems, through diagnosing safety and performance issues and delivering simulation-based intervention, irrespective of the location, modality or content of the simulation. It offers a functional alignment with quality improvement activities in healthcare institutions, while encompassing those educational interventions targeting practice behaviour or patient outcomes.
Translational simulation requires close relationships with clinical governance and quality improvement services in healthcare institutions and can be used effectively as part of comprehensive health service improvement strategies. Translational simulation activities encompass modalities, locations and delivery methods that address the gap between simulation education and patient outcomes.
Translational simulation, teams, and the EHR – ICE blog (royalcollege.ca)
For more information, visit the Ice Blog website.

The diagram above is based on the translational simulation cycle by Prof Victoria Brazil. Reference: Brazil, V. Translational simulation: not ‘where?’ but ‘why?’ A functional view of in situ simulation. Adv Simul 2, 20 (2017). See the online journal article Translational simulation: not 'where?' but 'why?' A functional view of in situ simulation.
About Simulation-based education (SBE) and simulation
What is a simulation?
Simulation-based education or SBE in healthcare is widely used in tertiary and postgraduate education and even with the community for life support training. It is "a technique (not a tool or technology) to replace, augment or amplify reality with guided experiences, often immersive in nature, that evoke or replicate substantial aspects of the real world in an interactive fashion". Simulation has a wide range of applications in healthcare for education, training and quality improvement. Using simulation to improve safety requires full integration of its applications into the routine structures and practices of health care.
What is in situ simulation?
In situ simulation takes place in the real patient care setting /environment such as birth centre, ED, wards, theatres to achieve a high level of realism and to test the environment to find latent or hidden threats.
In situ simulation is valuable to assess, troubleshoot, or develop new system processes. This type of simulation is particularly useful to ensure what is learned works in the actual space care is provided with the actual teams that will be providing it rather than in a simulation centre or lab where things may be quite different.

The Gandel Simulation Service is developing an extensive research and evaluation program, collaborating with University of Melbourne, Bond University as well as others examining the effectiveness of a translational simulation service across the Women's and Parkville precinct. Key research areas include:
- Teamwork and culture
- Maternity and newborn safety
- Gynaecology surgical skills
- Operating theatre teams
- Anaesthesia and emergency teams
- Obstetric trauma care
- Impact on quality and safety
- Procurement decisions
- Co-design of pathways, processes and
- Spaces
- Sustainability and cost effectiveness

The Gandel Simulation Service has links across the Parkville Precinct, with simulation activities involving numerous organisations, including the Royal Women’s Hospital, the Royal Melbourne Hospital, Peter MacCallum Cancer Centre and the University of Melbourne. The Gandel Simulation Service offers a range of support for educators and clinicians including development, implementation and evaluation of simulation activity.


Leading High Performance Teams Workshop
|
Delivering healthcare is complex. Trying to lead teams within our systems can feel frustrating and risks poor outcomes if we can't 'get it all together'. In this workshop, we'll think about what makes teams work - or not - in contemporary healthcare. At the end of the workshop, participants will:
Additional Online ResourcesTopic: Psychological Safety is No Accident
Watch this session on Vimeo. Topic: How human factors will save healthcare
Watch this session on Vimeo. Topic: Maternity Teamwork
Watch this session on Vimeo. |
Upcoming workshop date: TBC Please contact us by email for further details. Previous workshop dates: 10 October, 2022 9 March, 2022 7 March, 2022 21 September. 2021 |
GSS Simulated Birth Centre (with RANZCOG Basic Obstetric Skills Workshop) Program

|
A full-day program incorporating maternity emergency simulation and obstetric skill stations for maternity clinicians. Skills/topics include:
|
Upcoming dates - to be announced. Please contact us by email for further details. |
GSS Introduction to Fundamental Maternity Skills and Birth Program
Throughout 2022

|
A half-day orientation program is held each term for University of Melbourne medical students undertaking their Women’s Health placement at the Women’s. Includes orientation session to Birth Centre and Operating Theatre. Please contact us by email for further details. |

GSS COVID-19 PPH simulation video (including debrief at the end):

Infographics - These infographics are quick, easy-to-follow resources that cover the key themes and learnings from simulations at The Women’s.
Mental Rehearsal Cards - Mental rehearsal can be a critical element of improving individual and team performance in critical care settings. Developed to be used in a quick 5-8 minutes with your team.
Posters - Designed with a human factors approach, these PPE posters can be printed for use in your clinical area (A3 size recommended).
Clinical Care - Short and sharp 5-minute team debriefings using the below Guide can enable staff to share what went well, what could have been better, and what else was learned following an emergency.
The focus is on teamwork and systems improvement, not individuals. Psychological first aid or later debriefs may be needed in certain complex and distressing situations.
Here is the Clinical Care Debrief Guide (PDF, 734 KB) and a related video on Vimeo.