
https://www.thewomens.org.au/patients-visitors/pec-week-22
By now, you’ve probably had or are about to have your Booking-In appointment at the hospital.
Part 1: This stage in your pregnancy

Diabetes is a condition where there is too much glucose (sugar) in your blood.
Gestational diabetes mellitus (GDM) is a type of diabetes that can develop during pregnancy. It affects thousands of people and usually happens between weeks 24 and 28 of pregnancy.
Most people who develop GDM won’t have it after their baby is born. However, some will continue to have high blood glucose levels after having their baby.
GDM is diagnosed when blood glucose levels are higher than normal during pregnancy. For this reason, we recommend testing for gestational diabetes at 26 to 28 weeks of pregnancy (unless you already have diabetes). If you have risk factors for gestational diabetes, testing should be done earlier in your pregnancy.
For your glucose tolerance test you need to:
- bring your pathology slip with you to the hospital; you got this at your last appointment
- fast from midnight the night before your test, until your test is completed the next day. This means no eating, chewing gum, or smoking. You can only drink water during this time.
The testing process involves several steps:
- you’ll have your first blood test
- you’ll drink a glucose drink from our pathology department
- you’ll continue to fast and have 2 more blood tests - one an hour after having the drink and another an hour later.
This test takes about 2 hours. Please stay in the hospital until it’s finished.
For more information about gestational diabetes, please visit our website.
Part 2: Things to consider


You may feel very well during your pregnancy, or you may feel irritated or quite unwell. Most discomforts in pregnancy are normal and can be managed.
If you’re worried about your symptoms, talk to your midwife or doctor. You might need medicine or treatment. If your symptoms become severe, call the hospital immediately.
This section covers many common concerns during pregnancy.
Our fact sheet coping with common pregnancy-related discomforts has more information, including morning sickness, constipation, vaginal thrush, and more.
Our fact sheet Coping with common pregnancy-related discomforts has more information, including morning sickness, constipation, vaginal thrush, and more.
Sleep problems
Many things can affect your sleep during pregnancy and make it hard to fall asleep or stay asleep. They include:
- nausea (feeling like you might throw up or vomit)
- vomiting
- sore or tender breasts
- increased heart rate
- shortness of breath
- higher body temperature
- frequent trips to the bathroom at night
- leg cramps.
Read this information from the Sleep Foundation to learn more about sleep problems and tips to improve your sleep.
Dental care

It’s important to take care of your teeth during pregnancy. Changes in hormones can increase the risk of tooth decay and gingivitis (red, swollen gums that bleed easily). Gum disease or bacterial infections in the gums have been linked with babies being born prematurely or with low birth weight.
Having good dental health before getting pregnant means that you’re less likely to need dental treatments during pregnancy. If you have a dental emergency while pregnant, you might need to have an X-ray.
X-ray machines emit tiny doses of radiation focused on a specific area. They are generally safe in pregnancy. However, it’s always important to let your dentist know you’re pregnant.
If you’re pregnant and have a Medicare card, you won’t have to wait for dental care in Victoria.
To learn more about taking care of your teeth during pregnancy, read this information from the Australian Dental Association.
Vaccinations
Vaccines are medicines that help protect you and your baby from infections and diseases that can make you sick.
When you get vaccinated, your body builds immunity to protect you against specific germs, like bacteria or viruses. This is called immunisation.
Check with your doctor that your vaccinations are up to date. Important vaccines include measles, mumps, rubella (German measles), chickenpox, diphtheria, tetanus, whooping cough, influenza (flu), and COVID -19. Your doctor can order a blood test to check your immunity levels.
The National Immunisation Program Schedule lists the recommended vaccines from birth through to adulthood.
Getting vaccinated
During pregnancy, it’s recommended that you get vaccinated for flu, whooping cough, RSV, and COVID-19. These vaccines pass protective antibodies to your baby through the placenta, helping protect them after birth and during their first few months when they’re most vulnerable to serious illness.
- Flu - symptoms, such as a high temperature, may be harmful for you and your baby. You can get a flu vaccination before or during pregnancy, especially if you’re pregnant during flu season.
- Whooping cough - this vaccination is strongly recommended between weeks 20 to 32 to protect you and your baby. Getting vaccinated during your pregnancy will protect your baby during their first 6 months. Partners and close contacts should also consider getting vaccinated, as studies show that parents are often the main source of infection in babies with whooping cough.
- Respiratory syncytial virus (RSV) – is a common and very contagious virus that infects the airways and lungs. It can affect people of all ages, but babies and young children are most at risk of serious illness. If you’re pregnant, getting a single dose of the RSV vaccine is recommended between 28 and 36 weeks to help protect your baby. This vaccination is free during pregnancy. Babies who are most at risk of severe RSV may also be offered free immunisation for extra protection.
- COVID-19 – COVID-19 is more dangerous when you’re pregnant. The best way to reduce your risk is to get vaccinated. Evidence shows that vaccines are safe if you are pregnant, breastfeeding, or planning a pregnancy. You can receive a vaccine at any stage of pregnancy.
To learn more, read our fact sheets on whooping cough and pregnancy and flu.
You can also read the Australian Government's information on free vaccinations during pregnancy.
Work
It’s important to make sure your work environment and the work you do is safe for you and your pregnancy. If you’re worried about your job or your workplace, talk with a health professional.
If at any time your work role or workplace becomes unsafe, your employer should arrange alternative work activities for you. They should also support you if you return to work while breastfeeding.
Australia has laws to protect you from discrimination at work, including specific protections for pregnancy and breastfeeding. Knowing your rights can be helpful when discussing concerns with your employer.
For more information, visit these websites:
- Pregnancy and breastfeeding discrimination - Victorian Equal Opportunity and Human Rights Commission
- Parental leave - Fair Work Ombudsman
Travel by air or car
When travelling for any long distance by car, plane, boat, or train, drink plenty of fluids, move around and stretch your legs often.
Wearing seat belts
Always wear a seat belt, regardless of the stage of your pregnancy. Wearing a seat belt protects both you and your unborn baby if there is an accident. It’s illegal not to wear a seat belt unless you have a current medical certificate from your doctor.
When the seat belt becomes uncomfortable over your baby bump, wear the lower belt under it, as demonstrated in the Queensland Government video seat belt safety in pregnancy - belt below bump.
Air travel
The safest and most comfortable time to travel by air is during your second trimester (between 20 and 32 weeks) when you’re feeling your best and have the lowest risk of pregnancy complications like miscarriage or premature birth.
For domestic flights in Australia, avoid flying after 36 weeks.
If you plan to fly overseas after 32 weeks, you may need special permission from your doctor. Before making any travel plans:
- talk with your midwife or doctor about travel and any vaccinations you may need
- check with your airline and travel insurance about their pregnancy policies
- find out about the medical care available at your destination, as some countries may have limited healthcare services compared to Australia
- be aware of potential risks like disease or travel restrictions that could delay your return.
Air travel and deep vein thrombosis (DVT)
Air travel, especially during pregnancy, can increase the risk of deep vein thrombosis (DVT). This is a blood clot that forms in a deep vein, most often in your leg. You can lower your risk of DVT by:
- drinking lots of fluid, especially water, to stay hydrated
- wearing fitted knee-high compression stockings
- moving around regularly and doing frequent leg exercises to improve blood flow
- if you’re at high risk, your doctor may recommend medicine to prevent clots.
For more information, read the fact sheet travelling during pregnancy from The Royal Australian and New Zealand College of Obstetricians and Gynaecologists.
Hair dyes and hair removers
Research on using hair dyes during pregnancy is limited. Generally, they’re considered safe because very little hair dye is absorbed through the scalp. But if you want to be very careful, avoid using them in the first 3 months of pregnancy.
Here are some tips if you decide to dye your hair while pregnant:
- go to a hairdresser instead of doing it at home
- if you dye your hair at home:
- do it in a well-ventilated area to avoid breathing in the fumes
- follow the package instructions and do an allergy test first
- wear gloves or ask someone else to apply the dye for you.
Visit the Pregnancy, Birth and Baby website for more information about cosmetic and beauty treatments during pregnancy and breastfeeding.


During your pregnancy, we’ll talk with you about your plans to feed your baby. Your feeding choices and past experiences are important.
Whether this is your first baby, or you’ve fed other babies, you may have questions.
Our fact sheet, you're pregnant, so let's talk about feeding your baby, is a good place to learn about breastfeeding and why it’s recommended for you and your baby.
Breast milk provides all the nutrition your baby needs for the first 6 months of life. It continues to be a big part of their diet throughout the first year and beyond.
However, if you choose not to breastfeed or offer breast milk, or if you’re unable to, we’ll give you information and support about formula feeding options.
Accreditation
The Women’s is a Baby Friendly Health Initiative accredited hospital and follows the World Health Organization’s 10 steps for successful breastfeeding.

Skin-to-skin contact right after birth is important. Placing your baby on your chest in their first hour of life helps them adjust to their new environment. This contact also keeps their temperature, breathing, oxygen levels, and heart rate stable. And it encourages breastfeeding instincts.
Read our fact sheet skin-to-skin care with your baby for details on the benefits for both you and your baby. It’s available in English, Arabic, Chinese and Vietnamese.


Starting breastfeeding soon after your baby’s birth ensures your baby gets colostrum, the first breast milk.
Colostrum is full of important nutrients. It helps stabilise your baby’s blood sugar levels, boosts their developing immune system, and protects them from illnesses in their first few months.

Room sharing, also called rooming in, means keeping your baby with you in your sleeping room. During your stay at the Women’s, you and your baby will most likely stay together.
Having your baby in the same room helps you notice when they’re hungry, tired, or need a cuddle.
Rooming in, breastfeeding, and providing a safe sleep space can also reduce the risk of SIDS (sudden infant death syndrome. For more safe sleeping information, visit Red Nose Australia.
At the Women’s, Pepi Pods can be used. These special plastic tubs are used as an alternative to standard cots. They allow you to safely share your bed with your baby, including after a caesarean birth.
Part 3: Physiotherapy and exercise


Exercising within your limits is very good during pregnancy.
As your baby grows:
- your stomach muscles need to be strong to support your baby’s weight
- your leg muscles need extra strength so you can climb stairs and get in and out of cars
- your back needs to be strong to lift and carry
- your pelvic floor muscles must be strong and effective to prevent them from becoming stretched and weakened as your baby grows (more details in the next section).
The best exercises are ones you enjoy, involve moderate intensity (where you’re not breathless and can talk), and you can do most days of the week.
Exercise and being active helps you stay well, feel positive, and cope with the challenges of becoming a parent.
If you weren’t active before pregnancy, starting strenuous or vigorous exercise could be harmful to you and your baby. Talk to a health professional to find out what exercise is best for you.
Our physiotherapists specialise in the physical changes that occur during pregnancy. They can assess and treat pregnancy-related back and pelvic pain.
Stop exercising and contact the hospital if you experience any of these symptoms while exercising:
- dizziness
- bleeding from your vagina
- contractions
- pain
- unusual shortness of breath
- headaches or nausea
- decreased baby movements
- your waters break or you have a steady flow of clear, watery fluid coming from your vagina.
Visit our website for more information about exercise in pregnancy and our Physiotherapy Department.
You can also find other certified physiotherapists specialising in pelvic floor physiotherapy on the Continence Foundation of Australia Physiotherapy Group website.

Posture is how you hold your body when you sit or stand. Your posture changes during pregnancy.
As your baby grows, your belly gets bigger, shifting your centre of gravity. This can affect your posture and balance.
Without realising it, you may change how you stand, sit, and walk. It’s important to be aware of your posture and try to stand and sit tall, but not stiff. When standing, balance your weight evenly on both feet and relax your shoulders. Gently tighten your lower abdominal muscles to support your baby’s weight.

Staying active and understanding your pelvic floor muscles are important steps to prepare for labour.
The pelvic floor is a group of muscles and ligaments that support the bladder, uterus, and bowel.
The openings from these organs - the urethra from the bladder, the vagina from the uterus, and the anus from the bowel - pass through the pelvic floor. The pelvic floor muscles attach to your pubic bone at the front and your tail bone at the back, forming the base of your pelvis.
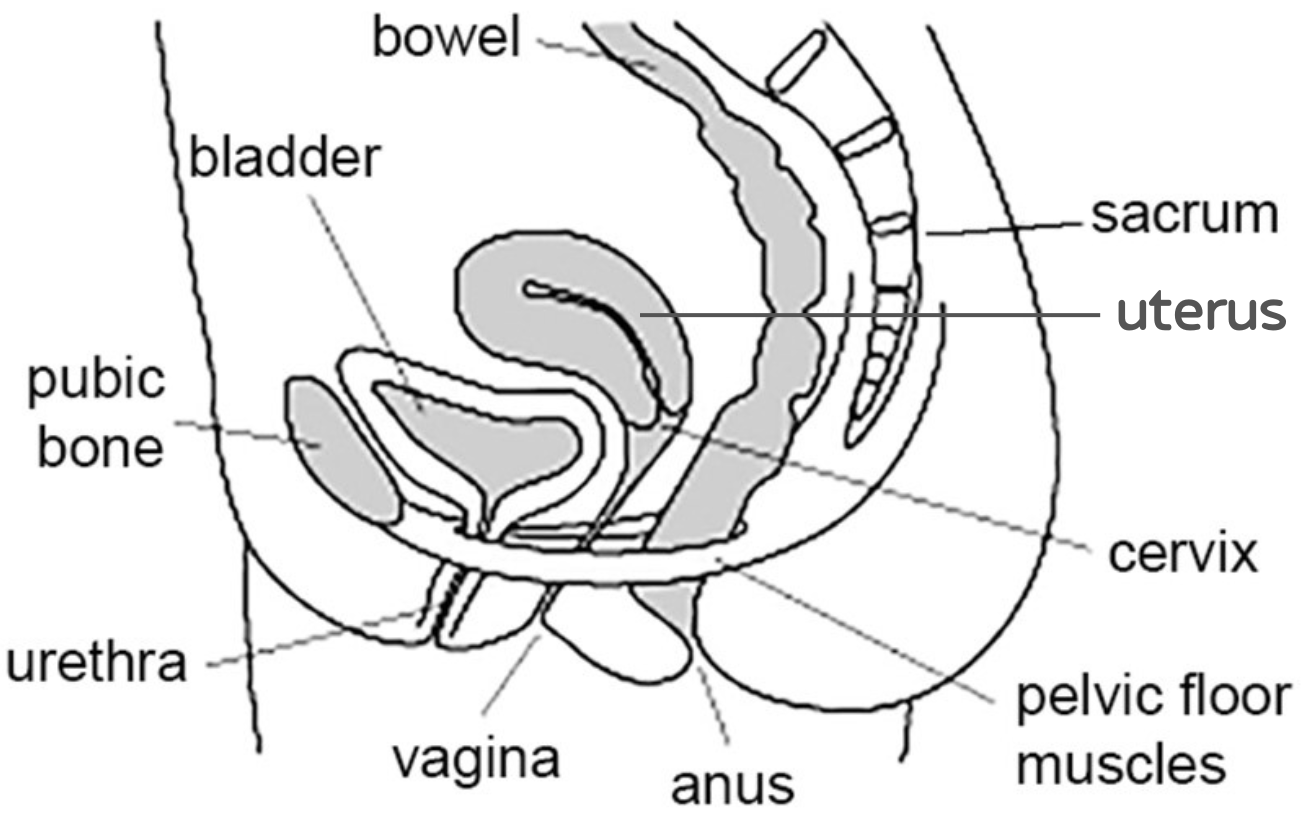
These muscles help hold your uterus in place and play an important role in sexual sensation and function.
Throughout pregnancy, they stretch and weaken due to your baby’s weight. Pregnancy hormones also loosen and stretch these muscles. It’s important to exercise them to keep them strong and working well.
You can also help prevent your pelvic floor muscles from weakening by avoiding constipation and straining on the toilet.
Watch our video to learn how to find and exercise your pelvic floor muscles.
Our pelvic floor exercises fact sheet provides more information about your pelvic floor muscles and is available in many languages.

Early in your pregnancy is the best time to learn how to relax. When you’re relaxed, your muscles loosen, and you can breathe more easily and smoothly. This keeps your oxygen levels high and your stress hormones low. Relaxation helps you cope with stress, tiredness, and pain.
Using relaxation methods in labour lowers your adrenaline levels. Adrenaline is a hormone your body produces in response to fear, anxiety, and pain. High adrenaline levels trigger our fight, flee or freeze response.
Relaxation increases the production of oxytocin, the hormone that helps labour progress. Being relaxed may also reduce the need for medical pain relief.
Learning breath awareness and relaxation techniques reduces anxiety and pain during labour and provides benefits after your baby is born.
Activities like pregnancy yoga, pregnancy Pilates, hypnobirthing techniques, walking, listening to music, tai chi, breath awareness, mindfulness, and mediation can help you relax.
To get the most out of these activities:
- find an activity that you enjoy
- practise as much as possible, at least 3 to 4 times a week, and when possible, practise with your birth support person.
The Centre of Perinatal Excellence website includes stress and relaxation strategies for pregnancy.

It’s normal to wonder if having sex could hurt your growing baby.
But if you have a healthy pregnancy and you want to have sex, there’s no need to worry - it won’t hurt you or your baby.
Everyone feels differently about sex during pregnancy. You might not feel like having sex at all. You may prefer cuddling, touch, or a massage instead. Or you might find you want more sex than usual.
As pregnancy progresses, sex may become more challenging. This can be a great time to get creative and try different positions together.
The most important thing is to listen to your body, do what feels right, and talk openly about what you need.
Always ask your midwife or doctor for advice if:
- you have any bleeding from your vagina - more blood than the size of a 50-cent coin
- you’ve had a miscarriage before
- your waters have broken (there may be a risk of infection to your baby)
- you’ve had a premature birth before or gynaecological problems.
For more information on sex during pregnancy, visit the UK National Health Service website and the Raising Children Network.

Now is a great time to talk with your partner or support circle about your needs during pregnancy, labour and birth, and after your baby is born.
Here are some ways they can get involved:
- attend clinic, doctor visits, and scans during pregnancy
- learn together by joining a Childbirth education program, reading fact sheets and other resources, and watching videos from the Women’s website
- talk about shared household responsibilities now and after the baby arrives
- discuss how your relationships may change when caring for a baby, especially in the first weeks and months. Pregnancy and parenting can bring many changes, so it helps to be prepared. You can find more information on the Australian parenting website, Raising Children
- start talking about your parenting expectations. Think about your family’s approach to parenting and the skills and behaviours you want to use or avoid
- discuss plans for returning to work and financial planning for at least the next 6 to 12 months. Find out about entitlements for parental leave and options for flexible working arrangements.
We hope you have found this information helpful.
If you have any health concerns please talk to one of your health care professionals – midwife, General Practitioner (GP), hospital doctor, etc.
There will be more to read and learn next week, in week 23 of your pregnancy. Stay safe and well.